
Nurse Practitioner (NP) Kelvin Bei has always believed that high quality primary care requires a patient-centred approach. “We want to automate what we can, but we also need to know our patients as people and take a holistic perspective. Are they falling through the gaps? Can we implement systems to prevent this moving forward?” When his clinic introduced HDC Discover, an application that provides access to community level trends in chronic disease management, Kelvin noticed something interesting. His diabetes monitoring rates were similar to colleagues in his region, but he saw an opportunity to elevate an already strong practice. “…the data in HDC Discover, from my colleagues at RISE, and NPs provincially, helped me realize that there was room for improvement. This provided the encouragement needed to undergo this QI project.”
Setting a Forward-looking Objective
Kelvin set a goal that aligned with evidence-based care:
Enhance the consistency of A1C, uACR and BP testing for patients with T2DM over the next 3 months, ensuring alignment with current provincial guidelines.
The guidelines emphasis:
- A1C testing every 3–6 months, depending on glycemic stability
- Annual uACR screening to detect early kidney changes
- Blood pressure, foot exams, and CV risk assessments incorporated into routine care
These were not just bureaucratic boxes to check – they were evidence‑based interventions that support long-term health and prevent complications; exactly the kind of proactive care Kelvin wants to champion.
Building a Better System
Kelvin approached the project with a systems lens rather than a personal one. He knew that even excellent clinicians benefit from reliable workflows.
He introduced several thoughtful improvements:
- EMR enabled patient communication, via emails
- Modified standing lab orders to simplify the ordering of recommended tests
- Team-based outreach empowering LPNs, RPHs, RNs & MOAs to help with chronic disease management and patient education.
- Clear, consistent patient education about why these tests matter
These changes weren’t about correcting deficiencies – they were about maximizing the use of available technologies and utilizing everyone’s strengths in a team-based care environment. Together, these changes created a more reliable system: one that didn’t depend on memory or chance.
Meaningful Outcomes
Within 3 months, diabetes visits felt more structured, more anticipatory, and less reactive. Patients felt cared for and appreciated the clarity and consistency. Gaps in care were identified and addressed through a team-based approach. “…maximizing each team member’s role and strengths allowed us to maximize our patients’ health potential.”
Not only did the change flow and feel better for the team, Kelvin saw measurable improvements in diabetes management across his panel, which further reinforced his objective to increase the quality of care provided to his patients:
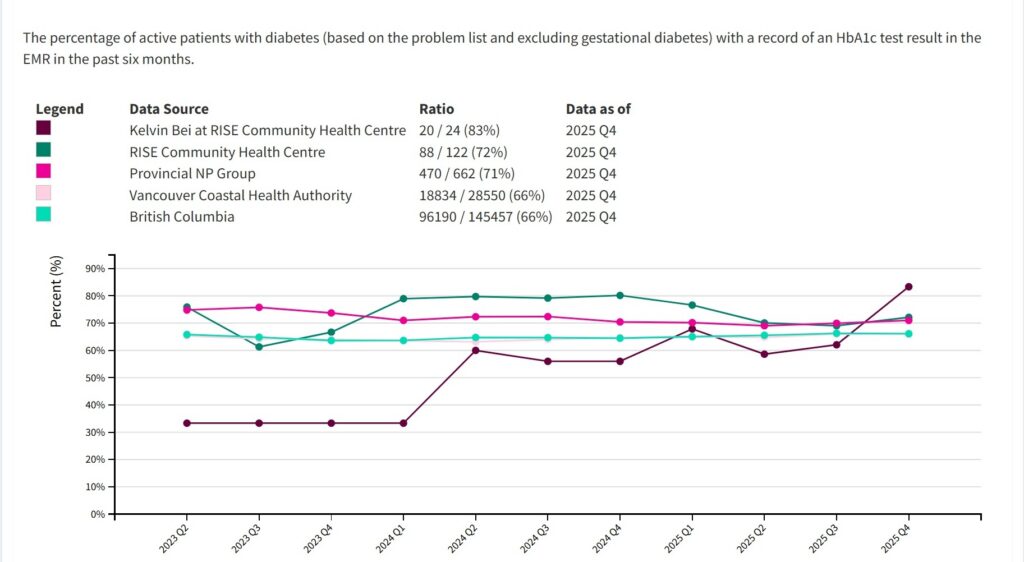
A 21% improvement in diabetes HbA1c monitoring and management.
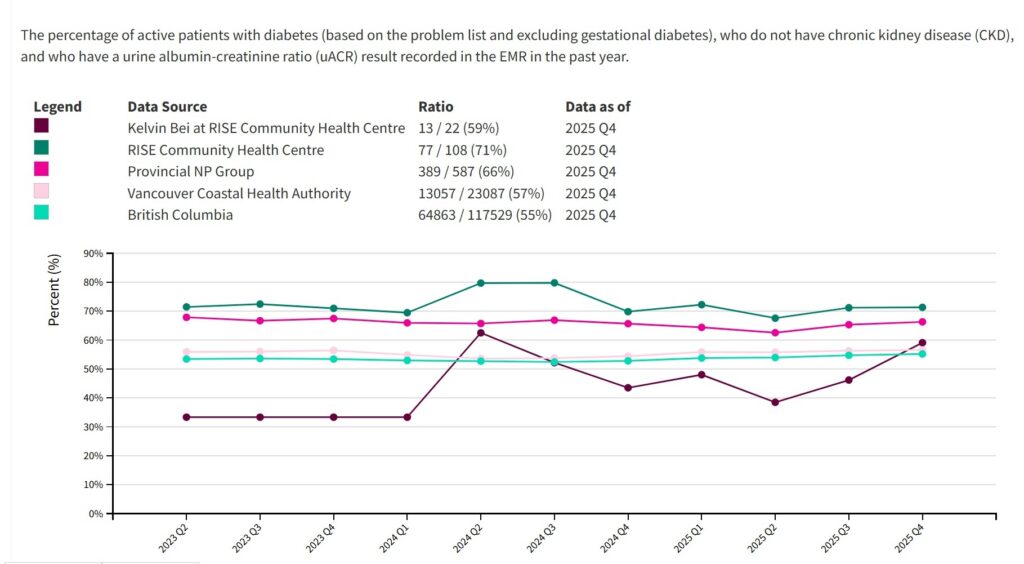
A 13% improvement in uACR monitoring and management for patients living with diabetes.
A 19% improvement in BP Management for patients living with diabetes.
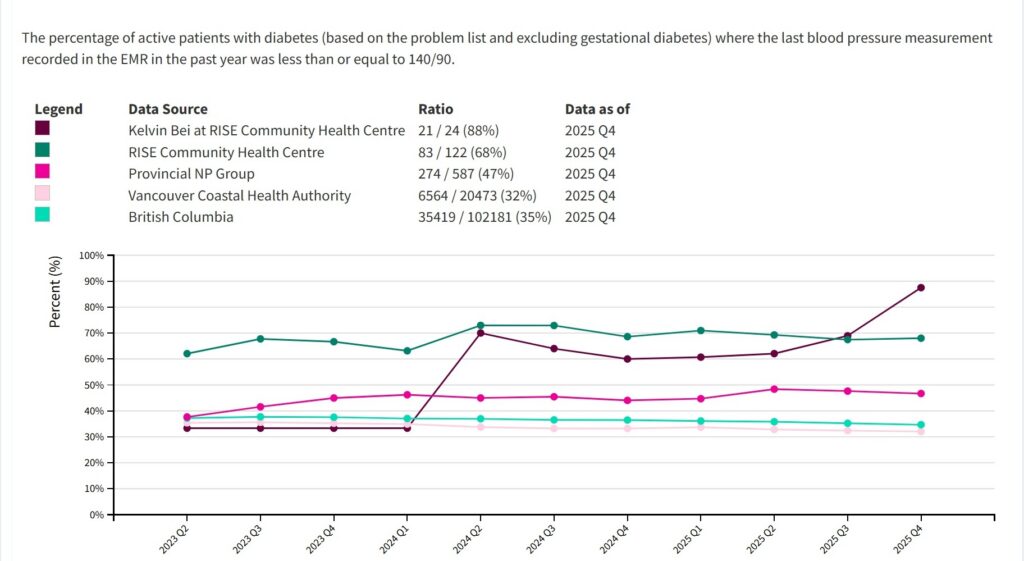
The visual feedback is highly reinforcing and motivating to the entire team. Going forward, the team will continue to monitor these measures to sustain their new systems. And if needed, they can decide whether there may be another opportunity to adjust clinic practices to continue to provide quality patient care.
Recognizing the Work: NNPBC Compensation
Importantly, NPs in British Columbia are supported to lead meaningful Quality Improvement (QI) as NNPBC provides compensation allowances for NPs who undertake QI initiatives. NPs can submit their QI activities online through the NNPBC compensation portal, ensuring they are reimbursed for the planning, data review, implementation, and evaluation work that goes into projects like Kelvin’s. Additionally, NPs can request participation in the ‘Provincial NP Group’ aggregate, as seen in the charts above. For further information on the group, please contact info@hdcbc.ca
This support signals a broader cultural shift: QI is not “extra”. It is a valued part of modern primary care providers and a key contributor to system-level improvement – and it deserves to be resourced accordingly.
“…the data in HDC Discover, from my colleagues at RISE, and NPs provincially, helped me realize that there was room for improvement. This provided the encouragement needed to undergo this QI project.“
Kelvin Bei,
Nurse Practitioner

A Model for Others
Kelvin’s story illustrates how quality improvement initiatives can emerge from curiosity, not crisis. It shows that even well-functioning practices can benefit from structured reflection and small, strategic changes. Whether it’s diabetes care, hypertension management, cancer screening, or mental health follow‑up, clinicians are choosing to invest the time to review and design workflows that strengthen their practice, empower their patients, and contribute to a more resilient healthcare system.
And with tools, guidelines, and compensation structures already in place, there has never been a better time for NPs to step into this work.
For other clinicians, it offers a simple invitation:
Explore your HDC Discover data. See what sparks your interest. And consider how a small change might strengthen your practice, your team, and your patients’ health.
Contact your HDC Clinical Services Manager at info@hdcbc.ca.