Heart failure is one of the leading causes of death in Canada and is a growing concern as it is also the leading cause of hospital admissions and readmissions across the country. With an aging population, the percentage of people suffering with chronic diseases, including heart failure, is expected to rise.
Current guidelines promote the use of guideline directed medical therapy (GDMT) to treat people with heart failure with reduced ejection fraction (HFrEF, defined by the American Heart Association as ejection fraction less than or equal to 40%), drawn from four classes of medications that have been shown to improve quality of life and life span for these patients.
HDC, working with Cardiologist Dr Daisy Dulay on a project sponsored by the Northern Interior Rural Division of Family Practice (NIRD) utilizing their Primary Care Network (PCN) Pharmacist, Michael Matula, developed a set of measures to support primary care providers in managing the treatment of patients with heart failure. Treatment of heart failure can be complicated by other chronic co-morbidities such as diabetes, hypertension, and chronic kidney disease. Using the skills of a trained pharmacist, in consultation with a cardiologist, to assist primary care providers in optimizing GDMT for patients living with heart failure, reducing the disease management burden resting solely on the primary care providers.
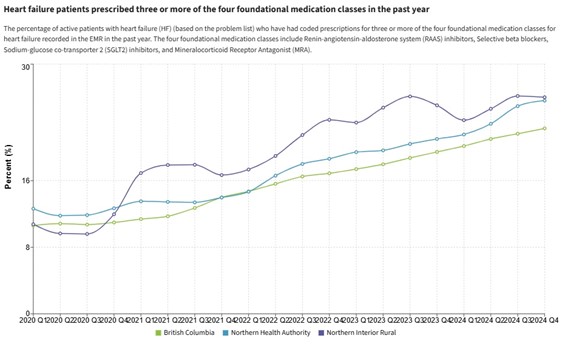
The gap is particularly evident in remote and rural areas where access to heart function clinics and specialists is not always an easy option. Of the clinics enrolled in HDC Discover across the province we see a rising curve, where increasingly patients with heart failure are being prescribed at least 3 of the 4 foundational medications available, topping at a rate of 22% for HDC’s provincial sample, representing approximately a quarter of primary care clinics. The project team is interested in tapping some collective energy to keep this trend going and improve both the quantity and quality of life for patients with heart failure.
Despite the gains in heart failure management with the introduction of new medications, the hospitalizations and mortality of patients living with heart failure remains high across the globe. As the population grows older, unstable patients living with heart failure will continue to contribute to high costs in managing exacerbations and hospitalizations. As heart failure advances, the burden on caregivers grows as they increasingly must assist with daily activities for their loved ones.
A recognized barrier to optimizing heart failure treatment is clinical inertia. Clinical inertia is defined as “the lack of treatment intensification in a patient not at evidence based goals for care” and it is postulated that three principal factors contribute to this inertia: system-related factors, provider-related factors and patient-related factors.
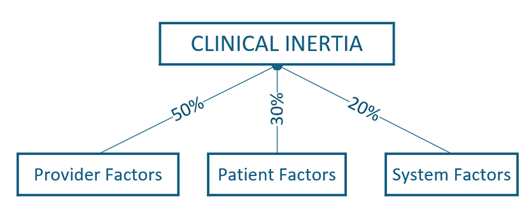
This project, aptly named, The Fantastic Four Heart Failure Project, aimed to address each of these principal factors by bringing together the patient, the provider, a cardiology specialist, and a PCN pharmacist to assist in optimizing heart failure treatment for patients within the NIRD catchment. Starting with a few providers in the region, providers were initially approached by their practice improvement coaches from the Practice Support Program (PSP) to assess their willingness to participate. Once permission was granted, the coaches reviewed practice data with the providers to find patients with heart failure with low ejection fraction, usually an element of an ECHO. This is where the system-related factors show up.
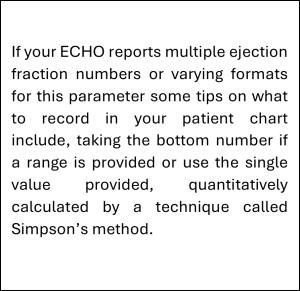
Many radiological and procedural reports that arrive in the inbox of the primary care providers do not routinely get parsed into structured fields within the Electronic Medical Record (EMR). As such, details contained within these reports are not readily available in the patient chart in a way that can be searched easily. Some elements of GDMT are suitable only for patients with heart failure that have low ejection fraction (EF), defined as less than 40%. Though the treatment options are expanding, one barrier can be special authority coverage and who prescribes them. For example, replacing the ACE inhibitor or angiotensin receptor blocker (ARB) with more effective Sacubitril/Valsartan requires proof of an EF of less than or equal to 40% and requires an internist or cardiologist to prescribe it initially. The first step for the providers is to identify which of their patients with heart failure have low ejection fraction. The Practice Improvement coaches can assist providers in optimizing their workflows to ensure these important details are captured as discrete data elements within the provider’s EMR. This system-related factor contributing to GDMT clinical inertia puts the manual data entry of ejection fraction burden on the already over-whelmed primary care office. Ideally, receipt of discrete results directly into the provider’s EMR would reduce the manual effort required to identify the population of focus: patients living with heart failure with a low ejection fraction.
Physician-related factors
The overwhelming medical information available today and challenges of keeping up with all the latest guidelines contribute to the physician-related factors of clinical inertia. For example, physicians may not be aware that SGLT2i medications can also be prescribed to patients with heart failure WITHOUT diabetes. Dapagliflozin, a SGLT2i, can be prescribed without special authority, unlike Empagliflozin. Dapagliflozin has added renal protection benefits.
In this project, once this cohort of patients with HFrEF are identified, the provider is invited to a triad meeting with the PCN Pharmacist and the Cardiologist to discuss treatment options and to gain consent for the patients to be seen by the PCN pharmacist on behalf of the provider. Originally, with consent of the patient and the guidance and support from the cardiologist, the PCN pharmacist books an appointment with the patient to review current treatments with an aim to optimizing GDMT and answer any questions or concerns the patient may have. In collaboration with the Rural Coordination Centre of BC (RccBC), the cardiologist can virtually meet with rural patients from the Northern Health region in collaboration with the family doctor or nurse practitioner while they are in the primary care office (RccBC’s C2C program). If there are opportunities to improve the care of the patient, a referral is made to the PCN pharmacist.
Patient-related factors
These hybrid meetings address the provider-related contributing factor to clinical inertia by upskilling the providers on GDMT for patients with heart failure and subsequent meetings between the pharmacist and the patients address the third factor by providing support and education for the patient directly. It is hard to convince a patient, when they are feeling well, why medications should be titrated. Time-crunched providers may elect to back off fine-tuning medications as it takes time to explain the rationale to continue to titrate heart failure medications. Having a pharmacist to work through the concerns that the patient and their caregiver may have and to take the time to explain why the medications should be titrated to maximally tolerated doses can help reduce the pushback. These pharmacist-led patient meetings are not as time-bound as primary care provider visits and allow for more information exchange with the patients, perhaps leading to a better understanding of the benefits of GDMT and ultimately better patient adherence to the treatment plans. Studies have indicated the optimal medical therapy can improve and extend a patient’s life by up to two years!
“Pharmacists, like physicians and nurse practitioners, prefer to use a shared decision-making approach to therapies. We know which agents and doses are best suited for optimal HFrEF management, based on evidence and the clinical presentation, and we engage the patient in a way that empowers them to choose which options are best for them. This often leads to greater satisfaction of care and improved adherence to prescribed therapies” Michael Matula, PCN Pharmacist, NH primary care pharmacist covering the Northern Interior Rural Division of Family Practice (NIRD).
While we have had a slower start than anticipated in NIRD due to physician turn-over, we continue to seek providers who have patients with heart failure and want to ensure they are optimizing their treatment to join our project.
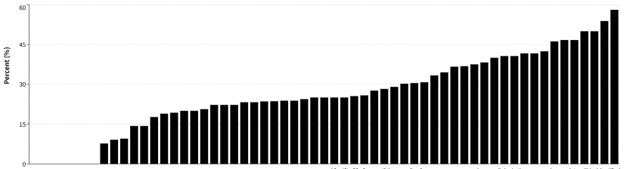
Among the primary care clinics registered with HDC within the Northern region, we see an average rate of 25.6% of eligible patients diagnosed with heart failure and prescribed 3 of the 4 foundational GDMT medication classes, with a range from 7.7 to 58% as of December 2024.
Rates of GDMT prescribing continue to rise across the Northern Interior region surpassing rates across the other regions within BC, although still for only a portion of those patients potentially eligible. Receiving discrete investigation results that can be queried within primary care clinic EMRs would reduce the administrative burden on these professionals and allow for simplified identification of patients that would benefit from medication optimization.
We encourage other Primary Care Networks (PCN) to utilize the PCN pharmacist resource to look into patients with heart failure and review their treatment plans to ensure they are optimized to the GDMT. HDC Discover has a series of measures to support this work, looking at rates of prescribing for each of the four individual classes, Beta Blockers, ACE Inhibitors, ARB and ARNI drugs from the RAAS class of medications, SGLT2 Inhibitors, and MRA medications. Review your own practice panels and find out where your patients may be further optimized to reach GDMT.

We thank NIRD for supporting this project with a project coordinator and the efforts of both Michael Matula, the PCN Pharmacist working with Dr Daisy Dulay, the Cardiologist for their foresight in identifying this gap in care and working to organize resources to support this project. Both have a keen interest in supporting high quality care in patients with heart disease, particularly addressing the patients who aren’t getting optimized medication treatment due to our overwhelmed healthcare system and long wait times to see specialists within the very busy heart function clinics across the province. This triad strategy will manage treatment for patients that either are discharged from a hospitalization event and awaiting to see a specialist or have seen a specialist and are awaiting treatment by a primary care provider. It is an example of how team-based care resources work to support the primary care provider. This project also exemplifies strong collaboration across three programs funded by the Family Practice Services Committee (FPSC) with Divisions, HDC and the Practice Support Program coming together to make this project work.
Where are you in this story? If you need support for identifying your patients with heart failure suitable for GDMT, we suggest starting a quality improvement project. PCN pharmacists interested in learning more can connect with HDC’s Manager of Community Engagement to get connected to this project’s PCN pharmacist for knowledge translation.